WHAT ABOUT SPINAL SURGERY?
In case you have not figured it out yet, the odds of you doing well after a Spinal Surgery are not exactly great. In fact, after you read this page, you will realize that they pretty well stink. And the odds of you improving after a second, third, or fourth surgery on your spine? They're in the toilet! A Vegas sports bookie would look at these odds and say, "Fuhhhhhget about it! " But I don't want you to take my word for it. This page is dedicated to showing you that you do not want to have a Spinal Surgery without exhausting every available option --- including Non-Surgical Spinal Decompression Therapy!
Ask any doctor worth his salt ---- any surgery is high risk. This is especially true of Spinal Surgeries because few people ever truly recover the quality of their life once they have gone under the knife. The brutal truth is that if you ask people who have had Spinal Surgery whether they would do it again, the answer is frequently "no". This is because such a large percentage of these people end up with even more problems than they started with. When compared to Non-Surgical Spinal Decompression Therapy, Spinal Surgery requires a longer recovery time, a longer and more difficult rehab, more missed time from work, frequently leads to permanent disability, and quite often a lifetime of NARCOTICS.
Spinal Decompression Therapy is radically different. It gets to the source of the pain by addressing it's cause ---- without all the invasive cutting, drilling, pinning, screwing, and wiring. The gentle "stretch / relax" pattern of the Non-Surgical Decompression pumps the disc. Since the Spinal Discs have no blood supply, this "pumping" action is critical for providing the disc with the things that would typically be supplied by the blood ---- water, OXYGEN, and nutrients to nourish the disc and restore it to health. The logarithmic pumping action of the Spinal Decompression Table helps take pressure off the discs, pressure off of the spinal cord, and pressure off of the Spinal Nerves. There is actually research indicating that Spinal Decompression Therapy CAN ACTUALLY REVERSE DISC HERNIATIONS AND INCREASE DISC HEIGHT. This can take pressure off of the SCIATIC NERVE as well as help relieve radiating pain into the arms.
The great thing about Non-Surgical Spinal Decompression Therapy is that there is no cutting, no anesthesia, and nothing inserted or installed in your spine that has the potential to cause infections. Nothing is wired, pinned, or screwed to the spine itself, and no bone is cut away or transplanted from cadavers. When compared to incredibly expensive Spinal Surgeries, Non-Surgical Spinal Decompression is tremendous bargain. And the really cool thing is that it is safe, gentle, relaxing, and EFFECTIVE as it expands the disc height while and improving range of motion. All of this helps to diminish nerve irritation and impingement .
WHY DO SO MANY PEOPLE OPT FOR SPINAL SURGERY IF THE OUTCOMES ARE SO POOR?
Most of it has to do with what they are told by a Neruo-Surgeon or Orthopedic Surgeon. There is an old saying that says, "if you are a carpenter and the only tool you have in your bag is a hammer, everything starts to look like a nail." There is no way to deny this effect. Surgeons, by their very job description, do surgery for a living. Now, I'm not saying that every Spinal Surgery is done for money, but how else do you explain a MORE THAN 800% INCREASE in the most dangerous and invasive Spinal Surgeries over the past dozen or so years ---- even though you will soon see that study after study after study says that these surgeries are ineffective, dangerous, and cause people to need additional Spinal Surgeries? Much of this mis-information seems to be coming from doctors who are telling desperate patients that.....
- Surgery is Your Only Option To Relieve the Terrible Pain (Rarely is this true. As you will soon see, large numbers of post-surgical patients are worse after surgery, and statistically most Non-Surgical Spinal Decompression Therapy patients have significant improvements in pain, range of motion, and the ability to perform day to day functions, that can be measured objectively.)
- Without Surgery, You Will Get Worse (Rather than debating this point, I would suggest that you speak with ten people who have already had the same Spinal Surgery that your doctors are pushing you to have. This statement is simply not based in reality, nor is it borne out by most of the research on Spinal Surgeries.)
ORTHOPEDIC SURGEON FOR CINCINNATI REDS PROFESSIONAL BASEBALL TEAM PROMOTES SPINAL DECOMPRESSION THERAPY

__"Although surgery may be suggested, there is no guarantee that it will help with the pain." Dr.
Timothy Kremcheck (like DR JAMES ANDREWS) has a reputation as one of the top orthopedic
surgeons in professional sports. Dr. Kremcheck is sought after by athletes from around the world to help get them back on the field after severe or debilitating injuries. As both the Medical Director and Orthopedic Surgeon for the Cincinnati Reds (not to mention he himself has had a back surgery), Dr. Kremcheck has a better understanding than most of us of the inherent dangers and risks of Spinal Surgery. "I've had back surgery, I had back surgery when I
was a young resident in orthopedic surgery and my back has been a
problem ever since because of the surgery and it's something that I wish
I could have turned back. I wish I would have had non-surgical
spinal decompression back then. It would have worked and so now I am
paying for it for the rest of my life."
KREMCHECK SAYS THE RISKS OF SPINAL SURGERY ARE ENORMOUS!
"With back surgery the risks are enormous. Things that go on and potentially go wrong with back surgery are enormous and they are life long, so anything that you can do non-operatively has got to be your first choice second choice and again multiple choices after that." Spinal decompression takes the disc from protruding and puts it back to the normal position and takes the pressure off of the spinal cord and the nerve roots and therefore takes a lot of the pressure and the spasm off of the musculature in the lower back, increases the range of motion, decreases the pain enhances the function of movement to do whatever you want to do..... If I have a patient that comes in, and they've got back pain or neck pain, before I would recommend that they have a surgery procedure or invasive procedure - even an epidural injection I would recommend the non-surgical disc decompression because there is no downside to trying this and it works"
KREMCHECK SAYS THE RISKS OF SPINAL SURGERY ARE ENORMOUS!
"With back surgery the risks are enormous. Things that go on and potentially go wrong with back surgery are enormous and they are life long, so anything that you can do non-operatively has got to be your first choice second choice and again multiple choices after that." Spinal decompression takes the disc from protruding and puts it back to the normal position and takes the pressure off of the spinal cord and the nerve roots and therefore takes a lot of the pressure and the spasm off of the musculature in the lower back, increases the range of motion, decreases the pain enhances the function of movement to do whatever you want to do..... If I have a patient that comes in, and they've got back pain or neck pain, before I would recommend that they have a surgery procedure or invasive procedure - even an epidural injection I would recommend the non-surgical disc decompression because there is no downside to trying this and it works"
NEVER CONFUSE SPINAL DECOMPRESSION WITH NON-SURGICAL SPINAL DECOMPRESSION THERAPY!
|
_Although Surgical Spinal Decompression and Non-Surgical Spinal Decompression Therapy sound alike in name, they share absolutely nothing in common with each other! Surgery is expensive, difficult to rehab, as well as known for creating unholy amounts of SCAR TISSUE in the underlying muscles, tendons, and ligaments. On top of this, it has a high rate of failures (you'll see this in a moment) that often require
additional surgeries. Sounds terrible doesn't it? It is. Especially considering that the second, third, and subsequent Spinal Surgeries almost always leave people worse off than they were before!
|
ADVANTAGES OF SPINAL DECOMPRESSION THERAPY COMPARED TO SPINAL SURGERY
Non-Surgical Spinal Decompression Therapy has been PROVEN EFFECTIVE for many people who have struggled with Spinal Disc problems ---- the same problems that many doctors would otherwise recommend surgery for. Seriously consider Spinal Decompression Therapy before jumping headfirst into a Spinal Surgery!
|
_
WHAT YOU CAN EXPECT IF YOU OPT FOR SPINAL FUSION SURGERY:
WHY THE NEED FOR ADDITIONAL SPINAL SURGERIES?
This is easily understood if you simply look at my DISC DEGENERATION PAGE. Each individual vertebrae and disc is created and designed to have a very specific range of motion. Too much or too little range of motion, and you will have problems --- big problems. However, these problems do not always occur right away (see previous paragraph). Surgeries on Spinal Discs must, by their very nature, significantly reduce the normal range of motion (plates, screws, bone grafts, and copious amounts of SCAR TISSUE & ADHESION tend to do this). When plates, pins, screws, wires, etc, are surgically anchored to the spine, this is the natural result ---- DECAY AND DEGENERATION OF THE SPINE AND DISCS. The discs that live both above and below the surgically altered disc(s), attempt to accommodate for this post-surgical loss of natural motion. This accommodation results in abnormal mechanical stresses to these adjacent spinal levels. Abnormal joint motion is the known cause of joint degeneration. But degeneration causes abnormal joint motion. Repeat ad infinitum!
WHAT YOU CAN EXPECT IF YOU OPT FOR SPINAL FUSION SURGERY:
- You have a 25% chance that the bone graft (taken from your hip or a cadaver) will not knit together. This will require another fusion to be performed.
- Any time that titanium or stainless steel is drilled, screwed, pinned, or wired into your skeleton / spine, the risk of infection skyrockets. In our current age of INEFFECTIVE & DANGEROUS ANTIBIOTICS, this is a bad place to be! Read about the death of All pro wide receiver, and later announcer JACK SNOW for the Los Angeles / St. Louis Rams Professional Football Team. He caught the infection from his hip replacement surgery.
- Less than 50% of Spinal Surgeries (including Spinal Fusions) do what they are advertised to do ---- take care of the pain and symptoms ---- Gulp.
- Recuperation and Rehab is a long and painful process.
- It is likely that your life will never be the same. This includes your work, your sex life, as well as your ability to play sports such as golf --- or even walk. Many people can no longer sit through church or a movie. Large numbers of those who have opted for these types of Spinal Surgeries are so bad that they can no longer pick up their grandchildren!
- Spinal Fusions last on average about a decade (8-12 years) before they cause severe enough DEGENERATION to the vertebrae and disc both above and below the fusion to require another Spinal Fusion Surgery. This process is likely to be repeated until they bury you.
WHY THE NEED FOR ADDITIONAL SPINAL SURGERIES?
This is easily understood if you simply look at my DISC DEGENERATION PAGE. Each individual vertebrae and disc is created and designed to have a very specific range of motion. Too much or too little range of motion, and you will have problems --- big problems. However, these problems do not always occur right away (see previous paragraph). Surgeries on Spinal Discs must, by their very nature, significantly reduce the normal range of motion (plates, screws, bone grafts, and copious amounts of SCAR TISSUE & ADHESION tend to do this). When plates, pins, screws, wires, etc, are surgically anchored to the spine, this is the natural result ---- DECAY AND DEGENERATION OF THE SPINE AND DISCS. The discs that live both above and below the surgically altered disc(s), attempt to accommodate for this post-surgical loss of natural motion. This accommodation results in abnormal mechanical stresses to these adjacent spinal levels. Abnormal joint motion is the known cause of joint degeneration. But degeneration causes abnormal joint motion. Repeat ad infinitum!
THE TRUTH ABOUT
"MINIMALLY INVASIVE"
SPINAL SURGERIES
??? MINIMALLY INVASIVE ???
Yeah, Right
Yeah, Right
_
"Minimally Invasive" Spinal Surgery is a misnomer ---- a term used to fool people into thinking that what the surgery they are about to have is not dangerous. Hey, it sure sounds better than things like "Open Spine Surgery", "Lamincectomy", or "Spinal Fusion" (all of which can be performed in a "minimally invasive" fashion . The truth is, it's all about the marketing. What does "Minimally Invasive Surgery" really mean? Only that the surgery was performed by entering the body through a small incision in the skin, a body cavity, or an anatomical opening, with the hopes of leaving the smallest amount of damage possible. Unfortunately, it does not always work as advertised.
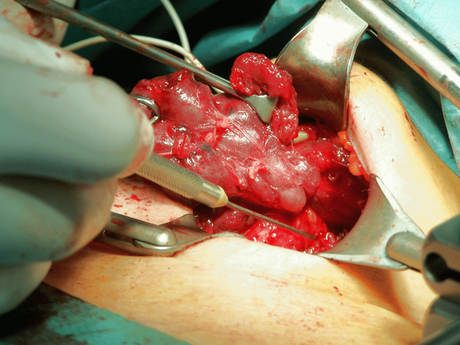
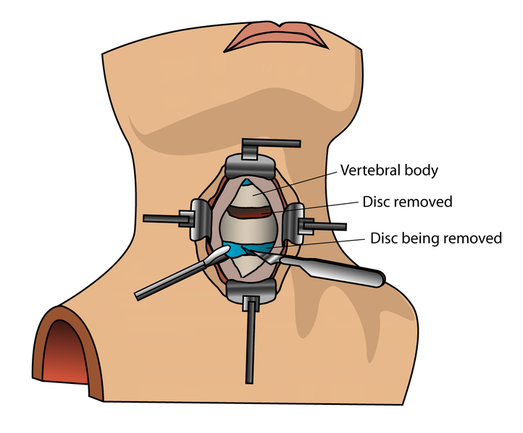
To gain access to the spinal column, mechanical spreaders (see picture above) are used to "stretch" spinal muscles out of the way. Remember that these are muscles that are already very tight / spasmed from the injured or damaged disc. The damaged disc between the spinal vertebrae is then cut out with a knife (see video below), or obliterated with a Class IV Laser or Dremmel-like drill. The decreased disc space is then expanded and a chunk of bone from the patients pelvis or a cadaver is put in its place. Because this mess is extremely unstable, metal brackets are anchored to the spine with titanium screws. This "Hardware" is mounted on the front of the problem vertebrae as well as the vertebrate above and below it. This "stabilizes" the spine while the body fuses the three vertebrae together over a period of 8-10 weeks. This procedure is medically termed Anterior Decompression & Fusion --- and the kicker is that it can be done in such a manner to meet the criteria to be called "Minimally Invasive".
"Minimally Invasive" Spinal Surgery is a misnomer ---- a term used to fool people into thinking that what the surgery they are about to have is not dangerous. Hey, it sure sounds better than things like "Open Spine Surgery", "Lamincectomy", or "Spinal Fusion" (all of which can be performed in a "minimally invasive" fashion . The truth is, it's all about the marketing. What does "Minimally Invasive Surgery" really mean? Only that the surgery was performed by entering the body through a small incision in the skin, a body cavity, or an anatomical opening, with the hopes of leaving the smallest amount of damage possible. Unfortunately, it does not always work as advertised.
To gain access to the spinal column, mechanical spreaders (see picture above) are used to "stretch" spinal muscles out of the way. Remember that these are muscles that are already very tight / spasmed from the injured or damaged disc. The damaged disc between the spinal vertebrae is then cut out with a knife (see video below), or obliterated with a Class IV Laser or Dremmel-like drill. The decreased disc space is then expanded and a chunk of bone from the patients pelvis or a cadaver is put in its place. Because this mess is extremely unstable, metal brackets are anchored to the spine with titanium screws. This "Hardware" is mounted on the front of the problem vertebrae as well as the vertebrate above and below it. This "stabilizes" the spine while the body fuses the three vertebrae together over a period of 8-10 weeks. This procedure is medically termed Anterior Decompression & Fusion --- and the kicker is that it can be done in such a manner to meet the criteria to be called "Minimally Invasive".
_
ENDOSCOPIC SURGERY
Sometimes a different type of Spinal Surgery is performed. Endoscopy involves inserting a probe between the spinal levels which can slice off the protruding portion of the disc that is contacting / irritating the nerve. This procedure is risky for several reasons. The HERNIATED DISC is usually is pressing directly on a nerve root. Any contact between a stainless steel surgical instrument and the nerve can cause varying degrees of instant and irreversible neurological damage. Also, since the goal of this surgery involves shaving / slicing off the herniation that is pressing on nerve tissue, the disc remains thin even after the surgery is complete. This "deflated" appearance is caused by a loss of the jelly center of the Spinal Disc (Nucleus Pulposus). Not only does loss of disc height lead do abnormal disc function (the known cause of DISC DEGENERATION), it frequently leads to immediate or eventual STENOSIS of the INTERVERTEBRAL FORAMEN. This means is that the small window-like opening where the Spinal Nerves exit the Spinal Cord, calcifies and shrinks.
ENDOSCOPIC SURGERY
Sometimes a different type of Spinal Surgery is performed. Endoscopy involves inserting a probe between the spinal levels which can slice off the protruding portion of the disc that is contacting / irritating the nerve. This procedure is risky for several reasons. The HERNIATED DISC is usually is pressing directly on a nerve root. Any contact between a stainless steel surgical instrument and the nerve can cause varying degrees of instant and irreversible neurological damage. Also, since the goal of this surgery involves shaving / slicing off the herniation that is pressing on nerve tissue, the disc remains thin even after the surgery is complete. This "deflated" appearance is caused by a loss of the jelly center of the Spinal Disc (Nucleus Pulposus). Not only does loss of disc height lead do abnormal disc function (the known cause of DISC DEGENERATION), it frequently leads to immediate or eventual STENOSIS of the INTERVERTEBRAL FORAMEN. This means is that the small window-like opening where the Spinal Nerves exit the Spinal Cord, calcifies and shrinks.
SPINAL LAMINECTOMY
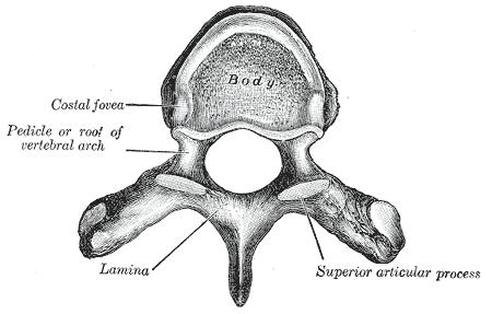
_A Laminectomy is the name of the operation that removes the part of the vertebrae called the lamina. The traditional form of Laminectomy (aka "Conventional Laminectomy") cuts away much more than just the lamina is
removed. The entire back part of the vertebrae, along with overlying ligaments and muscles, is removed. This "Surgically Decompresses" the spine, with the hope that it will take pressure off of the Spinal Cord and Spinal Nerves. Unfortunately, Laminectomies create lots and lots of instability --- which as we have already seen, leads to SPINAL DEGENERATION and invasive surgeries (SPINAL FUSIONS). The usual recovery
period lasts for months with a Conventional Laminectomy.
FAILED BACK SYNDROME (FBS)
AKA FAILED BACK SURGERY SYNDROME (FBSS)
AKA POST-LAMINECTOMY SYNDROME
_
Failed Back Surgery Syndrome (FBSS) is a condition that is characterized by persistent and unrelenting back or leg pain following Spinal Surgery. Contributing factors include but are not limited to residual or recurrent DISC HERNIATION, post-operative Spinal Nerve pressure, ABNORMAL JOINT MOBILITY, SCAR TISSUE, depression, anxiety, INSOMNIA and too little physical activity (de-conditioning). DIABETES, AUTOIMMUNITY, heart or artery disease and smoking also contribute to poor outcomes as well.
All sorts of "interesting" (desperate would better describe many of these) non-surgical treatments have been used in the past, and their track record is pathetic. These include things like Nerve Blocks, Transcutaneous Electrical Nerve Stimulation (TENS), Radio Frequency Ablation (burning out nerves with radio waves), Bio-Feedback, drugs of all kinds, especially NARCOTICS, membrane stabilizers, antidepressants, electrical spinal cord stimulation, CORTICO-STEROID INJECTIONS, and internal morphine pumps. For most people who have already had a back surgery, at least part of this list will look familiar. This is because many of these things were tried before your first back surgery.
Failed Back Surgery Syndrome (FBSS) is a condition that is characterized by persistent and unrelenting back or leg pain following Spinal Surgery. Contributing factors include but are not limited to residual or recurrent DISC HERNIATION, post-operative Spinal Nerve pressure, ABNORMAL JOINT MOBILITY, SCAR TISSUE, depression, anxiety, INSOMNIA and too little physical activity (de-conditioning). DIABETES, AUTOIMMUNITY, heart or artery disease and smoking also contribute to poor outcomes as well.
All sorts of "interesting" (desperate would better describe many of these) non-surgical treatments have been used in the past, and their track record is pathetic. These include things like Nerve Blocks, Transcutaneous Electrical Nerve Stimulation (TENS), Radio Frequency Ablation (burning out nerves with radio waves), Bio-Feedback, drugs of all kinds, especially NARCOTICS, membrane stabilizers, antidepressants, electrical spinal cord stimulation, CORTICO-STEROID INJECTIONS, and internal morphine pumps. For most people who have already had a back surgery, at least part of this list will look familiar. This is because many of these things were tried before your first back surgery.
WHY SO MANY BACK SURGERIES FAIL
America does more Spinal Surgeries than any country on the planet. One of the biggest reasons for our abysmal failure rate with Spinal Surgeries is that our medical community is not really following the guidelines that they themselves created. What are these guidelines, you might ask? Here are a few that were pulled directly from the website of Aetna Insurance Company. Other insurance companies (including Medicare) will have similar (if not identical) guidelines.
As long as there are not "emergency" issues present (cancer, fractures, aneurysms, etc) or spondylolisthesis, Aetna considers Spinal Surgery medically necessary when all of the following criteria are met:
WHAT IS CONSERVATIVE CARE?
If you read these guidelines for surgery -vs- no surgery, they beg the question of what constitutes "Conservative Care". After all, if you are supposed to try 6-12 weeks of it (or a year according to Duke University) before even thinking about having a Spinal Surgery, you had better have a good idea of exactly what it is. Again, here is the list that was put together by AETNA. It should be noted that CHIROPRACTIC ADJUSTMENTS are high on this list. Of course Aetna, like all other insurance companies that I am aware of (including Medicare), consider Spinal Decompression Therapy to be "Experimental ". Aetna's guidelines actually state, "For persistent non-radicular (SCIATICA) Low Back Pain with common degenerative changes (DEGENERATIVE DISC DISEASE), fusion surgery is superior to non-surgical therapy without interdisciplinary rehabilitation in 1 study, but no more effective than intensive interdisciplinary rehabilitation in 3 studies".
In the American Pain Society / American College of Physicians Clinical Practice Guideline on "Nonpharmacologic Therapies for Acute and Chronic Low Back Pain," Chou and Huffman (2007) reached the following conclusions: "Therapies with good evidence of moderate efficacy for chronic or subacute low back pain are cognitive-behavioral therapy, exercise, SPINAL MANIPULATION, and interdisciplinary rehabilitation."
SURGICAL FUN FACTS FOR BACKS
Here are a few tidbits that I pulled out of Aetna's long (very long) paper on Guidelines for Spinal Surgeries. Not surprisingly, some of the things that I found in the paper actually contradicted each other. Some of these are direct quotes, some are paraphrases to make difficult verbiage simpler.
As long as there are not "emergency" issues present (cancer, fractures, aneurysms, etc) or spondylolisthesis, Aetna considers Spinal Surgery medically necessary when all of the following criteria are met:
- All other sources of pain have been ruled out; and
- Imaging studies (e.g., CT or MRI) indicate nerve root compression that directly corresponds to the clinical findings of the specific affected nerve root; and
- Member has failed at least 6 weeks of conservative therapy (12 weeks with Spinal Fusion ---- Duke University says this should be a whole year); and
- Member's activities of daily living are limited by persistent pain radiating from the back down to the lower extremity (SCIATICA); and
- Physical findings of nerve root tension are present upon examination (i.e. positive SLR, Sicard's Test, Turyn's Test, etc); and
- Presence of neurological abnormalities (e.g., reflex change, sensory loss, weakness) persist on examination and actually correspond to the specific affected.
WHAT IS CONSERVATIVE CARE?
If you read these guidelines for surgery -vs- no surgery, they beg the question of what constitutes "Conservative Care". After all, if you are supposed to try 6-12 weeks of it (or a year according to Duke University) before even thinking about having a Spinal Surgery, you had better have a good idea of exactly what it is. Again, here is the list that was put together by AETNA. It should be noted that CHIROPRACTIC ADJUSTMENTS are high on this list. Of course Aetna, like all other insurance companies that I am aware of (including Medicare), consider Spinal Decompression Therapy to be "Experimental ". Aetna's guidelines actually state, "For persistent non-radicular (SCIATICA) Low Back Pain with common degenerative changes (DEGENERATIVE DISC DISEASE), fusion surgery is superior to non-surgical therapy without interdisciplinary rehabilitation in 1 study, but no more effective than intensive interdisciplinary rehabilitation in 3 studies".
- Avoidance of activities that aggravate pain (no kidding)
- CHIROPRACTIC MANIPULATION in the first 4 weeks (AMAZING STUDY). Aetna's paper contained this statement, "there is evidence that manual therapy, exercise and acupuncture are cost-effective management options compared with usual care for persistent non-specific low back pain."
- Cognitive support and reassurance that recovery is expected (THIS IS EQUALLY AS EFFECTIVE AS SPINAL SURGERY)
- Education regarding spine biomechanics (Sorry, THIS IS ALSO EQUALLY AS SPINAL SURGERY)
- Exercise / Stretching program
- Heat / Cold modalities for home use
- Limited bed rest with gradual return to normal activities (Bed rest needs to be very limited. Research shows that there is a direct correlation between longer periods of bed rest --- a medical treatment of choice just a couple of short decades ago ---- and the propensity to develop permanent dysfunction and disability.)
- Low impact exercise as tolerated (e.g., stationary bike, swimming, walking)
- Pharmacotherapy (e.g., non-narcotic pain relievers, NSAID'S, avoid MUSCLE RELAXERS, avoid NARCOTICS)
In the American Pain Society / American College of Physicians Clinical Practice Guideline on "Nonpharmacologic Therapies for Acute and Chronic Low Back Pain," Chou and Huffman (2007) reached the following conclusions: "Therapies with good evidence of moderate efficacy for chronic or subacute low back pain are cognitive-behavioral therapy, exercise, SPINAL MANIPULATION, and interdisciplinary rehabilitation."
SURGICAL FUN FACTS FOR BACKS
Here are a few tidbits that I pulled out of Aetna's long (very long) paper on Guidelines for Spinal Surgeries. Not surprisingly, some of the things that I found in the paper actually contradicted each other. Some of these are direct quotes, some are paraphrases to make difficult verbiage simpler.
- About 90% of the population will experience Low Back Pain in their lifetime. In America, Low Back Pain is the number two reason for doctor visits behind Upper Respiratory Surgeries (HERE).
- The role of Advanced Imaging (CT, MRI) in non-specific acute low back pain should be limited.
- Physical findings (examinations) and MRI findings correlate poorly with symptoms (HERE).
- MRI'S ARE OVERUSED.
- An MRI is appropriate only for people who have failed conservative care, including a combined physical and psychological treatment program, and are considering a referral for an opinion about Spinal Fusion.
- The exact cause of Low Back Pain can only be identified in about 15% of the cases (HERE).
- It is unclear if methods for identifying specific anatomic sources of back pain are accurate (HERE).
- The most common causes of Low Back Pain are due to HERNIATED DISCS, PROLAPSED DISCS, SLIPPED DISCS, SPINAL STENOSIS, & something called SPONDYLOLYSIS (a fancy name for DEGENERATIVE DISCS) (Lehrich and Sheon, 2007).
- Conservative care without immediate imaging is considered appropriate for patients with SCIATICA, as long as symptoms are not bilateral or associated with urinary retention / loss of bowel control (Ibid).
- [Concerning Spinal Surgeries], average benefits are small for function and moderate for pain. Furthermore, more than half of the patients who undergo surgery do not experience "excellent" or "good" outcomes. Although operative deaths are uncommon, randomized trials show that early complications occur in approximately 18% of patients who undergo Spinal Fusion Surgery (HERE).
- Different fusion procedures, including anterior lumbar interbody fusion, posterolateral fusion, posterior lumbar interbody fusion and transforaminal lumbar interbody fusion, and anterior-posterior combined fusion, do not vary significantly in pain or disability outcomes, although there are differences in complication rates.
- Increased stiffness from the insertion of screws and rods has been hypothesized to lead to increased DEGENERATION AT SPINE SEGMENTS ADJACENT TO THE FUSION.
- The effectiveness of lumbar fusion with posterior transpedicular screws, was compared to the effects of exercises on 60 patients aged 25 to 60 years with Low Back Pain lasting longer than 1 year after previous surgery for disc herniation. The program consisted of a lecture intended to give the patient an understanding that ordinary physical activity would not harm the disc and a recommendation to use the back and bend it. This was reinforced by three daily physical exercise sessions for 3 weeks. The primary outcome measure was the Oswestry Disability Index (ODI). The success rate was 50% in the fusion group and 48% in the exercise group. The authors concluded that for patients with chronic Low Back Pain after previous surgery for disc herniation, lumbar fusion failed to show any benefit over cognitive intervention (advice) and exercise.
- After Dr. Mizra led his team in a major analysis of studies comparing Cognitive Therapy (advice) to Spinal Surgery, the authors concluded that surgery may not be more efficacious than structured cognitive-behavior therapy (ADVICE EQUALLY AS EFFECTIVE AS SPINAL SURGERY).
- Even though there have been all sorts of "technological breakthroughs" in surgical methodology, these have not changed outcomes of Spinal Fusions at all (DEYO). We know also that since this study was done, there is evidence showing that Spinal Fusions have increased by between 800-1,000%.
- The same study said that Common complications of Spinal Fusion Surgery includes instrument failure (7%), complications at the bone donor site (11%), neural injuries (3%), and failure to achieve a solid fusion (15%). In addition, fusion is known to cause increased rate of disc degeneration in spinal segments above and below the site of fusion.
- In a 2003 review of the literature on Failed Lumbar Spine Surgeries, DR DIWAN & TEAM estimated that 10%-15% of patients who have undergone a Surgical Spinal Decompression Surgery and 15%-20% of patients who have had a spinal fusion procedure for DEGENERATIVE DISC DISEASE of the lumbar spine, undergo additional Spinal Surgery within 3-5 years due to significant back and leg symptoms. The rates go up from there. By the way, numerous studies have stated that surgery should not be performed on DEGENERATIVE DISCS.
- When doing studies on Spinal Surgeries, it is interesting to note that most surgeons come to the conclusion that Spinal Surgeries are safe and effective. However, most of the medical research experts and Ph.D's who later review these studies for large meta analysis's, conclude just the opposite.
_The Washington State Guidelines on Spinal Fusion
_The Washington State Department of Labor and Industries (2004) cited
the following as relative contraindications for lumbar fusion:
- Current evidence of a factitious disorder (malingering / faking it).
- Current smoking
- Greater than 12 months of disability benefits prior to consideration of fusion
- High degrees of somatization on clinical or psychological evaluation (Somatization disorders are long-standing conditions in which a person has physical symptoms that involve more than one part of the body, but no physical cause can be found. FIBROMYALGIA is frequently classified as such.)
- Multiple levels of DEGENERATIVE DISCS in the lumbar spine
- No evidence of functional recovery (return to work) for at least 6 months following the most recent spine surgery
- Presence of a personality disorder or major psychiatric illness
- Psychosocial factors that are correlated with poor outcome, such as history of drug or alcohol abuse
- Severe physical de-conditioning (you're out of shape --- something a huge number of Americans deal with).
|
www.DoctorSchierling.com
www.DestroyChronicPain.com www.DestroyTendinitis.com www.DestroyPiriformisSyndrome.com www.BBTMO.com www.DestroyObesityToday.com www.ColdLaserCure.com www.SpinalDecompressionMissouri.com www.DestroyFibromyalgia.com www.EndoGut.com www.ThyroidEpidemic.com www.DestroyMigraineHeadaches.com |
GENERAL INFORMATION
SCAR TISSUE REMODELING: CHRONIC PAIN WE FIX TENDINITIS / TENDINOSIS PIRIFORMIS SYNDROME / PAIN IN THE BUTT BRAIN-BASED THERAPY WEIGHT LOSS & OVER ALL HEALTH COLD LASER THERAPY IS HOT! NON-SURGICAL TREATMENT OF DISCS THERE IS HOPE FOR YOU IMMUNE & ENDOCRINE SYSTEM / GUT THYROID EQUALS METABOLISM HEADACHES STEAL YOUR LIFE |