Do You Really Want That "New" Artificial Disc Procedure You Read About on the Internet?
It looks like it should be so simple. "Hey Doc, why can't they just insert a rubber bushing in there where the disc should be?" Let me explain to you a couple of reasons that these artificial discs have never worked well in the past, are not working well in the present, and will most-likely never work well in the future.
- HYDRAULICS
The disc is an avascular tissue. This means that it has no blood supply. When you think about the things that blood provides your cells (oxygen, nutrients, water) as well as the things it removes (toxicity, acidity, metabolic waste products), you will start to realize that for a disc not to have a blood supply is a big deal ---- a really big deal.
So, if the disc has no blood supply, how in the world does it get the things into the disc that it needs to live, and then get rid of the waste products? The ever-amazing Spinal Disc acts as its own pump. If the disc is moving / functioning properly, everything works as it should. When the disc pumps, the blood-like exchange of nutrients, water, and oxygen ---- for waste products, takes place via the fluid that is pumped in and out of the disc. And the Spinal Discs stay healthy! But if the Spinal Discs do not move properly, bad things begin to happen, and the exchange taking place between the fluid and the ligamentous tissues of the disc becomes increasingly diminished.
- SPINAL COMPLEXITY AND PROXIMITY TO NERVES & SPINAL CORD
I will not belabor this point, but just understand that the spine and nerve system is complex. No, that is a gross understatement. The spine and nerve system are absurdly complex. When surgeons go in and start cutting, chiseling, stapling, screwing, wiring, bolting, drilling, pinning, sawing, and who-knows-what-else, you not only end up with a boatload of SCAR TISSUE, you end up with a literal grab-bag of potential side effects and problems ---- frequently permanent! I understand that there is a time and place for spinal surgery. However, even some of the most respected Neurosurgeons in the business claim that these surgeries are about 500 times more common than they should be (HERE).
WHY WOULD YOU NOT TRY CONSERVATIVE METHODS LIKE SPINAL DECOMPRESSION THERAPY FIRST?
I ask this question every time I talk to a patient who has already had 2 or 3 spinal surgeries, but is telling me that they will do absolutely anything I tell them to if I could just help relive some of their pain. You may have already heard this because its been in the news for the past several years, but several medical studies have confirmed that rehabilitation for low back pain works just as well as disc replacement surgery (read that again and let it sink in). Recently, publishing in the British Medical Journal (BMJ), researchers added to the evidence for effective rehabilitation, stating that the results are similar to surgery but without the risks. It's still a roll of the dice; the only difference is that if conservative methods do not work, you are not out anything but time and money (approximately 2-3% of the cost of a Spinal Fusion). Spinal Decompression Therapy may not always work, but it's not going to ruin your life!
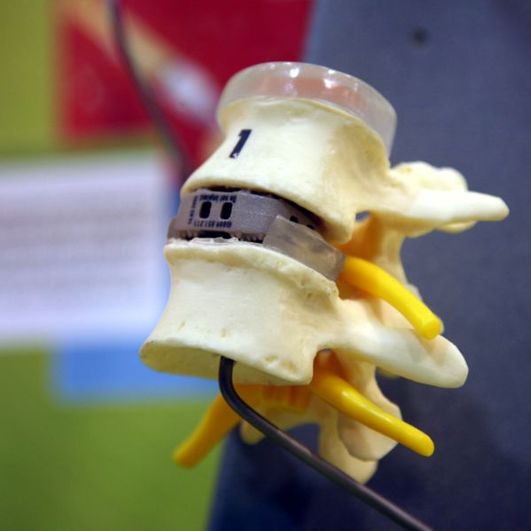
Disc replacement surgery involves removing DEGENERATIVE DISCS or HERNIATED DISCS and replacing them with Titanium or Stainless Steel endplates and a polymerized core whose purpose is to "try" and act like the soft and pliable Nucleus Pulposus of a Spinal Disc. As you might imagine, neither bone nor hardened metals have the ability to act similarly to the jelly of the nucleus!
More risks? Another recent study published in the prestigious British Medical Journal (BMJ) stated that the risks of Disc Replacement Surgery are "enormous", including:
•A re-operation rate of 5-10%,
•Vascular injury rate of 5-10%
•Possible amputation due to vascular injury
And that's in the first year! As time goes on, the problem gets worse. When questioned, most doctors will admit that even "successful" Spinal Fusions only last about a decade before wearing out the discs above and below the surgery!
GULP!
Other well known risks include: allergies to the material the fake disc is made from, breaking the fake disc, failure for the whole mess to actually fuse once the fake disc is implanted, slippage can occur that will dramatically alter biomechanics, and on and on and on. This does not even get into the problem of repeat surgeries. When two vertebrae are fused, there is abnormal motion (too little) at the fusion. However, there is also now abnormal motion at the discs above and below the fusion site (too much motion). Unfortunately, abnormal motion is the chief cause of DISC DEGENERATION. This is why Spinal Fusions (which themselves create seriously abnormal mechanical function of the disc) actually create the need for repeat Spinal Surgeries ---- fusions at the levels both above and below the surgically altered discs. Which itself creates further abnormalities of motion. It's that vicious cycle again! But hey, if you're a Spinal Surgeon, it's great job security!
Then there is a significant chance of nerve or spinal cord injury, as well as the common surgical risks associated with anesthesia and infection. If you think that the threat of infection is not real with a fusion (plates, pins, wires, and screws are implanted in your spine), go online and see what the medical community is saying about the infection rate for people who are having stainless steel or titanium implanted permanently into their bodies! My brother (an MD) thought he was going to have to have a Spinal Fusion, and the thought terrified him. Why? The threat of infection when metal is surgically implanted into the human body.
SPINAL DECOMPRESSION THERAPY FOR THOSE SUFFERING WITH CHRONIC SEVERE SPINE PAIN
Why should a person with chronic low back pain consider Spinal Decompression Therapy for their low back or neck? Our experience as well as the experience of millions of patients world-wide prove that Spinal Decompression Therapy is a great alternative to surgery for many chronic low back or neck pain patients. It carries almost no risk, and typically patients START SEEING RESULTS EARLY IN THE PROGRAM! In short, surgery not only misses the root problem, it often messes people up and leaves them wondering what to do and where to turn. Don't be "that person".
If this blog hits pretty close to home, my best suggestion for you would be to call Tracy and set up an appointment for a free consultation with Doctor Schierling. If you are a candidate for Spinal Decompression Therapy, he will tell you. IF YOU ARE NOT, he will tell you that also. Call (417) 934-6337 today.






 RSS Feed
RSS Feed